3D surgical planning for tracheal stenosis treatment
- MIRAI 3D
- 26 may 2021
- 2 Min. de lectura
Dr. Pablo Pérez Castro & Rubén Valenzuela
Hospital San Juan de Dios - Santiago de Chile, Chile
Benefits
✔ Improve understanding of anatomy and the relationship between different structures.
✔ Define the surgical approach
✔ Provide increased safety for surgeons
✔ Improve treatment results
✔ Enrich communication with the patient
✔ Provide a consultation tool within the operating room
Clinical Case
A 60 year old male patient comes to the clinic with stridor and desaturation in relation to ambient oxygen.
He has a history of prolonged intubation for cardiogenic shock and coronary stenting 8 months prior to the consultation. He is also hypertensive and a former smoker.
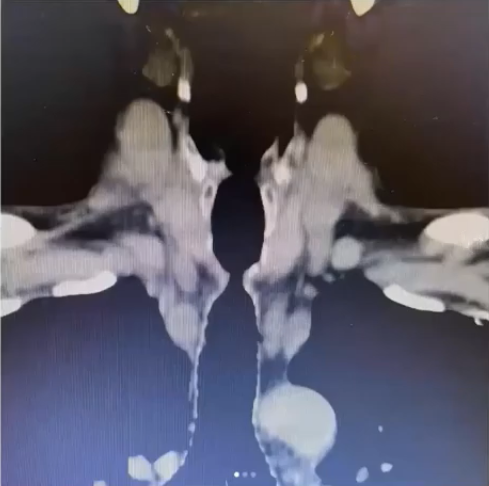
As he was stable, a CT scan of the neck and thorax showed a fairly severe subglottic stenosis behind the sternal manubrium.
An emergency rigid bronchoscopy was then performed, where it was determined that there was a concentric stenosis of approximately 5mm in diameter. Dilatation with an 8.5mm bronchoscope was performed.
For the surgical team, the definitive management of the patient was then under discussion. One option was to perform rigid bronchoscopy on demand and the other was to perform a tracheal resection.
In the first instance, due to his morbid history, a conservative procedure was chosen. The patient was dilated on three occasions: the first was the same as the emergency procedure; the second was with corticosteroid infiltration and the last with mitomycin C. The patient returned to the institution for further treatment. The patient returned to the institution approximately every 1 month.
In this context, it was decided to proceed with surgical treatment with tracheal resection for which a 3D biomodel was requested to plan the surgery.
3D anatomical model
◾ FDM Technology
◾ Material: PLA
◾ Resolution: 0.2 mm
◾ Finish: One colour
Surgical planning and outcomes in the operating room
To define the treatment details, Dr Pérez Castro's surgical team relied on a virtual model and a physical 3D biomodel. The surgeons recognised that the digital and physical modelling of the patient's pathology clearly showed the stenosis, its concentric shape and its relationship with the cricoid cartilage and the sternal ridge. Furthermore, its dimensions could be identified and measured, and the stenosis was small but not so extensive, around 1.5 cm.

For them, it was very important to know the exact location of the narrowing, as this would influence the approach they would choose. When they saw the 3D model, they confirmed that the stenosis was directly behind the sternum, so they could resect via the cervical approach without the need to open the sternum.

Finally, the procedure chosen and performed was an anterior cervicotomy with tracheal resection, followed by tracheal anastomosis, which was performed with good results by Dr. Valenzuela, head of the thoracic surgical team.
Dr. Perez, regarding his experience with anatomical 3D models, believes that "In non-specialised airway centres, i.e. low volume, 3D models can be a relatively inexpensive way to minimise complications and improve surgical outcomes".
You may be interested in: "3D Chest - Narrowing resection margins and achieving a more economical surgery". Dr. Matías Nicolás at the Hospital Privado de Comunidad (Mar del Plata, Argentina) had 3D anatomical models that allowed him to perform a minimally invasive approach.